16 Types of Healthcare Software in 2026
Contents
According to an industry forecast by Meticulous Research, the healthcare IT market is expected to grow at 13.8% CAGR (Compound Annual Growth Rate) to 2027, to reach a value of $511 billion.
However, as the report was published before the coronavirus outbreak, these numbers could potentially be even higher, with healthcare apps becoming more and more popular during the pandemic.
The healthcare ecosystem is evolving with the integration of various software solutions designed to serve individuals, groups, and enterprises. In the following article, we’re going to guide you through the top 13 types of healthcare software present on the market. We’ll showcase examples of popular medical software developed and used by institutions, as well as healthcare apps used by individuals concerned about their health and well-being.
Sixteen of the most popular types of healthcare software
1. Electronic Health Record (EHR) Software
EHR software is one of the most popular (if not the single most popular) type of software used by hospitals and clinics. In many ways, it’s similar to a CRM, only adjusted to the medical industry. EHR software provides clinical solutions that support healthcare providers in making informed decisions by offering evidence-based products tailored for various users, including individuals, groups, and enterprises.
EHR software collects information on patients – for example, the medication they take, doctors’ recommendations, and the procedures that they have undergone in the past.
Many programs also include a financial module for invoicing and payment, and a separate portal for the patient, which allows patients to access their consultation history, medical records, and prescriptions. EHR software contributes to improved patient outcomes by providing comprehensive patient data that enhances patient care quality.
The two most popular types of EHR software are:
- Electronic patient record software (EPR) – used internally by hospitals to store and process their patient information.
- Electronic medical record software (EMR) – used to store data like medication types and dosage, past and planned procedures, and data on the patient’s recovery course.
Examples: eClinicalWorks, Allscripts
2. Medical database software
Similarly to Electronic Health Record software, medical database software stores patients’ histories and treatment plans. However, unlike in EHRs, the database is categorized by disease, not patients’ profiles.
Medical database software helps doctors in two key areas:
- Making better treatment decisions by cross-referencing a patient’s case with similar cases.
- Educating themselves by reviewing clinical cases of a given disease.
By enabling doctors to make more informed treatment decisions, medical database software can lead to better health outcomes.
A dermatologist can, for example, use this type of software to browse all patients diagnosed with Atopic Dermatitis and compare their symptoms, treatments, and recovery plans.
3. Medical research software
Medical research software is used for two primary purposes: education and sharing research with the medical community. This type of software is commonly used to train medical personnel and to support diagnoses if no similar clinical cases among patients can be referenced internally.
Additionally, medical research software can improve financial outcomes by streamlining research processes and reducing costs.

Image source: PubMed
Example: PubMed.gov
4. Medical diagnosis software
Medical diagnosis software for doctors allows them to exchange anonymized patient records so that they can fill any informational gaps preventing them from providing an accurate diagnosis. This type of software often leverages artificial intelligence (AI) to analyze all available patient data and generate probable diagnoses.
There are also medical diagnosis apps available for individuals. Such apps allow users to check if their symptoms require a visit to hospital. Diagnosis apps like these have become popular during the COVID-19 pandemic. By providing accurate and timely diagnoses, medical diagnosis software significantly enhances the overall patient experience.
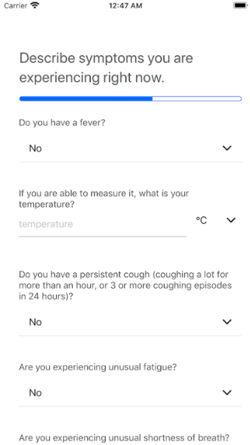
Source: Google Play Store
Examples: Human DX, OSP Labs, COVID Symptom Tracker
5. Medical imaging software
Medical imaging and visualization software is used primarily for processing MRI/CT/PET scans and designing 3D models.
Medical 3D imaging software permits:
- Human anatomy 3D modeling. Such programs let medical technicians create tailored models for individual patients. For example, 3D modeling software is used to generate and print out a real-life model of a patient’s teeth before a planned orthodontic treatment.
- Designing and printing equipment or body parts. This software is used to print elements of medical equipment or body parts, like artificial limbs or coronary stents needed for cardiovascular surgery.
Examples: Materialise, Vepro
6. E-prescribing software
More and more countries around the world are switching to electronic prescriptions, which also means e-prescribing software is becoming a must-have for doctors.
The software lets medical professionals track, renew, and cancel prescriptions for their patients. It’s also integrated with national drug reference databases.
Example: MediTab
7. Telemedicine software
Telemedicine is truly a booming industry, with a market value expected to reach $64 billion by the year 2025 – and that’s just the data for the United States alone! What makes it so successful is its convenience for both doctors and patients.
Telemedicine software enables healthcare professionals to conduct appointments with patients online, either through a web browser or a mobile app. In some software, the video conferencing feature is complemented by e-prescriptions and a billing module.
Examples of telemedicine applications: Doxy.Me, ZingTree
8. Appointment scheduling (booking) software
Booking software helps hospitals, clinics, and medical practices manage their appointment systems online. Typically, the software features a patient panel that lets individuals schedule appointments via an app or website.
Often, it also has an email notification system and automatic reminders for doctors and patients about upcoming appointments.
Example: SimplyBook.Me
9. Medical billing software
This software helps hospital accounting departments keep track of patient invoices, payments, and any other financial operations. It’s often integrated into bigger systems, such as EHR or hospital management software.
Example: Epic Care
10. Hospital management software
Hospital management software assists hospital administration in day-to-day operations. These types of programs usually help with the automation of accounting, medical billing, claims, out-patient management, inventory, bed management, and others.
Hospital management software often integrates with EHR software to help simultaneously keep track of patient records.
Example: Availity
11. Medical equipment management software
The goal of this type of software is to relieve hospitals and medical practices of manual stocktaking and equipment maintenance.
Medical equipment management software supports the sound functioning of clinics with features like automatic maintenance scheduling and inventory alerts.
Example: Sortly
12. Health tracking apps
In 2019, the global mHealth (short for ‘mobile health’) app industry was valued at $37 billion.
A large portion of the market can be attributed to the following app categories:
- Fitness – for example, the popular 8fit app.
- Diet – for example, Fitatu Calorie Counter and Diet.
- Meditation and stress reduction – for example, the incredibly popular Calm and Shine apps.
There’s also an increasing number of apps that integrate with IoT devices worn to source and analyze users’ health data. Some of the most popular types are wristbands for sleep tracking (for example, FitBit), jewelry (for example, the health-tracking Oura Ring), glucometers, and thermometers (used, amongst other things, for menstrual cycle tracking – for example, the Kindara app).
13. Personal Health Record software (medical diaries)
Unlike health tracking apps, the majority of which are used to maintain a healthy lifestyle, Personal Health Record software serves a different purpose – monitoring diseases.
These types of software serve as medical diaries – and can be either held on the patient’s device or integrated with the doctor or hospital’s software.
A great example that demonstrates how Personal Health Record software works is the Tulipa app, designed for patients suffering from Parkinson’s disease. In the app, the patients note down any symptoms, sensations, medication, or treatment, and can generate a health report before their next doctor’s visit.
This type of software can support the patient towards recovery, or alert medical staff on the worsening condition of a patient as soon as the first symptoms appear.
14. Remote Patient Monitoring (RPM)
Remote Patient Monitoring (RPM) has revolutionized the healthcare industry by providing the ability to collect patient data outside of traditional healthcare institutions like clinics and hospitals. This cutting-edge technology enhances the depth of patient health information available and even facilitates remote diagnoses based on collected data. Much like telemedicine services, RPM technology experienced significant growth during the pandemic, as traditional health management processes were disrupted.
RPM technology includes a variety of devices, such as heart rate and blood pressure monitors, wearable ECG monitors, and meters for measuring glucose and blood oxygen levels. By enabling real-time monitoring and alerting doctors or clinics of any detected abnormalities, remote patient monitoring software plays a vital role in providing quality healthcare.
Especially beneficial for individuals with chronic diseases, post-surgery recovery patients, and the elderly, RPM technology and devices have significantly improved the efficiency and efficacy of in-home healthcare services. The continued evolution of remote patient monitoring systems is set to drive a new era in patient care, making health management more accessible and efficient.
15. Mobile health (mHealth) apps
Initially perceived as disruptive by some healthcare practitioners, mHealth apps have now become an indispensable part of modern healthcare services. These intuitive applications empower patients by simplifying administrative tasks such as settling medical bills, scheduling appointments, and facilitating virtual consultations with nurses or doctors. High-performing mHealth apps provide patients with seamless access to a range of telehealth services.
A standout feature of these innovative mHealth apps is their integration with EMR/EHR software systems. With the necessary patient consent, healthcare professionals can effortlessly access pertinent medical records during a virtual consultation. This seamless flow of information enhances efficiency by enabling swift sharing of data for referrals, prescriptions, and other crucial aspects of patient care.
When effectively integrated with local or international healthcare infrastructure, mHealth apps represent a positive disruption in the healthcare industry. They redefine the ways in which patients access their healthcare, setting new standards for digital healthcare solutions.
16. Laboratory Information Management Systems (LIMS)
LIMS are specialized software solutions designed to manage various aspects of laboratory operations. They assist in tracking samples, managing associated data, and ensuring compliance with regulatory requirements. In healthcare, LIMS play a vital role in clinical laboratories by:
-
Sample Management: Efficiently tracking patient samples from collection to analysis, reducing errors and improving turnaround times.
-
Data Management: Storing and managing large volumes of laboratory data, facilitating easy retrieval and analysis.
-
Regulatory Compliance: Ensuring that laboratory processes adhere to industry standards and regulations, which is critical for patient safety and data integrity.
By integrating LIMS, healthcare providers can enhance laboratory efficiency, improve data accuracy, and maintain high standards of patient care.
Digital acceleration in healthcare in 2025 and beyond: Enhancing Clinical and Operational Efficiency
It’s safe to say that the healthcare software market is in full blossom. No wonder; the digitalization of healthcare brings many benefits – improved efficiency, cost reduction, and better control of finances and patient data. With the increasing digital acceleration of medical services around the globe and a growing user base of health-tracking apps online, the industry is likely to grow. This digital acceleration is also expected to lead to improved health outcomes by enhancing the efficiency and effectiveness of healthcare delivery.

